Bimonthly internal assessment
DECEMBER ASSESSMENT:
"This is my submission for the Bimonthly internal assessment for the month of November."
Most of the information here have been collected from different reference sites, the links to which have been mentioned. The points copy pasted have been put in quotes.
The questions to the cases being discussed can be viewed from the link below 👇
https://medicinedepartment.blogspot.com/2020/12/medicine-question-paper-for-december.html?m=1
1) A 55 year old man with Recurrent Focal Seizures
Detailed patient case report here: http://ushaindurthi.
1. What is the problem representation of this patient and what could be the anatomical site of lesion ?
Ans :
55 year old man presented to the casualty with the complaints of Unable to move his right upper limb
he suddenly started complaining that he couldn’t move his right upper limb few minutes later he developed a sudden onset, tonic clonic seizures involving his right upper limb and lower limb lasting for 2 minutes following which he had another 8 episodes of focal seizures involving his right upper limb and right lower limb with a 2 minutes of gap between each episode. During these episodes he had uprolling of eyes
ANATOMICAL LOCATION :
Anatomical location is mostly due to acute infarcts Left frontal and parietal Cortex.
And also chronic infarct With gliosis changes in right parieto occipital focal gliotic focus Left occipital lobe.
Mild cerebral and cerebellar Atrophic changes with chronic ischemic changes.
Chronic lacunar infarcts right corona , caudate nucleus and bilateral thalami.
2. Why are subcortical internal capsular infarcts more common that cortical infarcts?
Ans: Multiple mechanisms have been proposed as the etiology of lacunar infarction. The usual etiology of small lacunar infarctions (between 3 mm and 7 mm) is lipohyalinosis of the small perforating arteries feeding deep subcortical structures. Another mechanism is micro-atheroma formation at the origin of penetrating arteries from major cerebral arteries like the middle cerebral artery, Circle of Willis, or the distal basilar artery. These first two mechanisms are proven pathologically and likely due to chronic hypertension and resulting in small vessel disease.
If the size of lacune is larger than 5 to 7 mm, it is often not caused by occlusion of 1 or 2 lenticulostriate arterial branches but from an atherothrombotic lesion involving the mainstem middle cerebral artery. These infarcts are named striatocapsular infarcts by Bladin and Berkovic.
Other proposed mechanisms that have been failed to be proven pathologically include tiny emboli causing obstruction and cerebral arteriolar and capillary endothelial dysfunction leading to small vessel disease as a result of extravasation of blood products.
Out of all the causes of Lacunar strokes, hypertension is the most common modifiable risk factor for stroke. For every 10mm hg decrease in blood pressure, there is a 1/3rd lowering of stroke risk in primary prevention. So it is extremely important to control the blood pressure effectively to prevent future strokes. Cigarette smoking doubles stroke risk.
https://www.ncbi.nlm.nih.gov/books/NBK534206/
Since the internal capsule is a very compact structure consisting of many neural pathways of diverse functions, not only the location of the lesion but also its size should be important factors affecting the patient's clinical symptoms
3. What is the pathogenesis involved in cerebral infarct related seizures?
Ans: Poststroke seizures can occur soon after the onset of ischemia or can be delayed. Many clinical studies make a distinction between early and late seizures based on differences in their presumed pathophysiology. Early poststroke seizures are thought to result from cellular biochemical dysfunction leading to electrically irritable tissue.2,3 Acute ischemia leads to increased extracellular concentrations of glutamate, an excitatory neurotransmitter that has been associated with secondary neuronal injury.2,4 Recurrent epileptiform-type neuronal discharges can occur in neural networks of surviving neurons exposed to glutamate.5 In addition, transient peri-infarct depolarizations have been observed in the penumbra after experimental occlusion of the middle cerebral artery.6,7 Other investigators failed to confirm this phenomenon in humans.8 There is a correlation between the number and the total duration of depolarizing events and infarct volume in the setting of ischemia,9 perhaps due to reductions in capillary perfusion leading to more profound ischemia in penumbral tissue.10 Experimental data also suggest that epileptogenesis is enhanced by hyperglycemia at the time of ischemia.11
In contrast to early-onset seizures, late-onset seizures are thought to be caused by gliosis and the development of a meningocerebral cicatrix.12 Changes in membrane properties, deafferentation, selective neuronal loss, and collateral sprouting may result in hyperexcitability and neuronal synchrony sufficient to cause seizures.13,14 Pronounced neocortical neuronal hyperexcitability was found in primary somatosensory neurons of rats 10 to 17 months after transient forebrain ischemia.
https://www.ahajournals.org/doi/full/10.1161/01.str.0000130989.17100.96
4. What is your take on the ecg? And do you agree with the treating team on starting the patient on Enoxaparin?
Ans: ST depressions noted in precordial leads V1 to V6
NSTEMI
Yes , i agree with the treating team on starting the patient on Enoxaparin.
https://www.sciencedirect.com/science/article/pii/S0735109702029017
5. Which AED would you prefer?
If so why?
Ans: As it is focal seizure i would prefer carbamazepine
And lorazepam / diazepam to prevent the conversion of focal seizure to GTCS
Antiepileptics https://pubmed.ncbi.nlm.nih.gov/28661008/
Atorvastatin https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6036014/
Aspirin https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6206448/
Enoxaparin https://www.sciencedirect.com/science/article/pii/S0735109702029017
Question 2) 55 year old man with Recurrent hypoglycemia
pt suddenly complained of giddiness , profuse sweating with grbs- 34 mg/dl
2. What is the cause for his recurrent hypoglycemia? And how would you evaluate?
Ans: The cause of his recurrent hypoglycemia is secondary to OHA's(glimi M1) ... And also glimi m1 is mostly cleared by renal and the patient also has increased creatinine ( AKI) ... Glimi is not excreted and continuously causing hypoglycemia..
3. What is the cause for his Dyspnea? What is the reason for his albumin loss?
Ans:
4. What is the pathogenesis involved in hypoglycemia ?
Ans :
5. Do you agree with the treating team on starting the patient on antibiotics? And why? Mention the efficacies for the treatment given.
Ans : Yes i agree with the treating team starting antibiotics as his renal parameters are deranged and he may be having AKI (?renal)
CUE / urine cultures / USG abdomen are not available to support it as renal cause of AKI
Spot urine sodium is high may be secondary to ATN
Case details here: https://
1. How would you evaluate further this patient with Polyarthralgia?
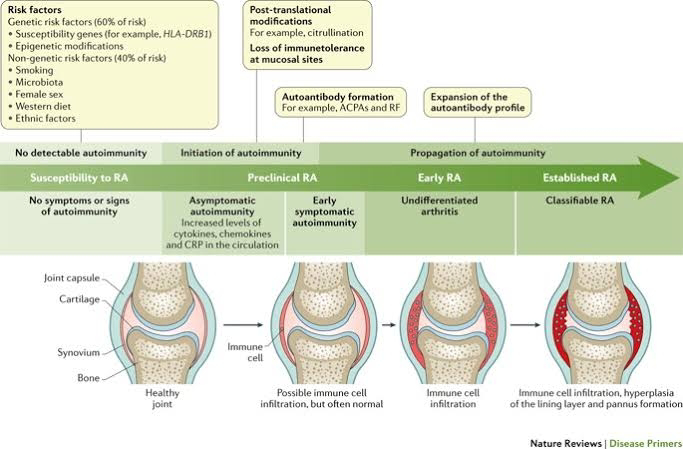
2. What is the pathogenesis involved in RA?
Ans:
3. What are the treatment regimens for a patient with RA and their efficacies?
Ans:
A total of 67 randomized controlled trials with 20,898 patients met the inclusion criteria. Most of the therapies presented better performance than conventional DMARDs (cDMARDs) and placebo in ACR20, ACR50 and ACR70. Conversely, the safety of cDMARDs and placebo seemed to be superior in AEs and SAEs. Also, tocilizumab (TCZ) and TCZ + methotrexate (MTX) showed better remission in pain compared to other treatments. Overall, certolizumab pegol (CZP) + MTX and TCZ + MTX had higher probability than the other treatments in efficacy outcomes.
Efficacy and safety of various anti-rheumatic treatments for patients with rheumatoid arthritis:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6348345/
3 (B)
75 year old woman with post operative hepatitis following blood transfusion
Case details here: https://
1.What are your differentials for this patient and how would you evaluate?
Ans:
-Transfusion related acute hepatic injury (TRAHI)
-Post transfusion hepatitis
-Ischemic hepatitis
coombs testing
antibody panel testing
- Piptaz & clarithromycin : for his right upper lobe pneumonic consolidation and sepsis
- Egg white & protien powder : for hypoalbuminemia
- Lactulose : for constipation
- Actrapid / Mixtard : for hyperglycemia
- Tramadol : for pain management
- Pantop : to prevent gastritis
- Zofer : to prevent vomitings
Case report here: https://appalaaishwaryareddy.
Serologic tests for hepatitis B surface antigen (HBsAg) and hepatitis B core antibody (anti-HBc) immunoglobulin M (IgM) are required for the diagnosis of acute hepatitis B virus (HBV). HBsAg is positive in both acute and chronic HBV infection; however, the presence of IgM anti-HBc is diagnostic of acute or recently acquired infection.Antibody to HBsAg (anti-HBs) is produced after a resolved infection and is the only HBV antibody marker present after vaccination. The presence of HBsAg and total anti-HBc, with a negative test for IgM anti-HBc, indicates chronic HBV infection; the absence of IgM anti-HBc or the persistence of HBsAg for 6 months indicates chronic HBV infection. The presence of anti-HBc alone might indicate acute, resolved, or chronic infection or a false-positive result.
A positive result suggests not only the likelihood of active hepatitis but also that the disease is much more infectious, as the virus is actively replicating.
HBV DNA testing is also recommended when occult HBV is suspected (positive anti-HBc and negative antibody to HBsAg [anti-HBs] and HBsAg) or in cases in which all of the serologic tests are negative.
REFERENCE:
[Guideline] Centers for Disease Control and Prevention. 2015 Sexually transmitted diseases treatment guidelines. Viral hepatitis. Centers for Disease Control and Prevention. Available at https://www.cdc.gov/std/tg2015/hepatitis.htm.
3. What is the pathogenesis of the illness due to Hepatitis B?
Ans:
4. Is it necessary to have a separate haemodialysis set up for hepatits B patients and why?
Ans:
Yes , separate machines must be used for patients known to be infected with HBV (or at high risk of new HBV infection). A machine that has been used for patients infected with HBV can be used again for non-infected patients only after it has been decontaminated using a regime deemed effective against HBV because of increased risk of transmission due to contamination.
https://pubmed.ncbi.nlm.nih.gov/12955683/
5. What are the efficacies of each treatment given to this patient? Describe the efficacies with supportive RCT evidence.
Ans:
Lactulose : for prevention and treatment of hepatic encephalopathy. https://pubmed.ncbi.nlm.nih.gov/27089005/
Tenofovir : for HBV
Octreotide : for upper GI bleed.
Lasix : for fluid overload (AKI on CKD)
Vitamin -k : for ? Deranged coagulation profile (PT , INR & APTT reports not available)
Pantop : for gastritis
Zofer : to prevent vomitings
Monocef (ceftriaxone) : for AKI (? renal)
6) 58 year old man with Dementia
Case report details: http://jabeenahmed300.blogspot.com/2020/12/this-is-online-e-log-book-to-discuss.html
1. What is the problem representation of this patient?
Ans:
58 year old weaver occasional alcoholic c/o slurring of speech , deviation of mouth to right side associated with drooling of saliva , food particles and water predominantly from left angle of mouth and smacking of lips since 6 months.
Urinary urge incontinence since 6 months.
Forgetfulness since 3 months.
He has delayed response to commands.
Dysphagia to both solids and liquids since 10 days.
K/c/o CVA 3 years back and now he was diagnosed as neuro degenerative disease - Alzheimer's (? Vascular - post stroke sequale)
2. How would you evaluate further this patient with Dementia?
Ans:
3. Do you think his dementia could be explained by chronic infarcts?
Ans:
Yes.. His dementia could be explained by chronic infarcts....
https://www.ninds.nih.gov/Disorders/All-Disorders/Multi-Infarct-Dementia-Information-Page#:~:text=Multi-infarct%20dementia%20(MID),occur%20without%20noticeable%20clinical%20symptoms.
4. What is the likely pathogenesis of this patient's dementia?
Ans:
Post stroke dementia
(1) Neurotoxicity, including dysregulated glutamate and calcium signaling, and neurotransmission imbalance contribute to synaptic dysfunction and neuronal loss
(2) Glia activation, including microglia and astrocytes, interfere with immunological processes in the brain further promoting non-resolving inflammation and neurodegeneration
(3) Tau phosphorylation and neurofibrillary tangle formation;
(4) Aβ plaque formation are key hallmarks of the AD brain. Specialized pro-resolving mediators and strategies aimed at boosting resolution such as using omega-3 polyunsaturated fatty acid exert differential effects on these targets and provide anti-inflammatory and pro-cognitive effects in neuroinflammation/degeneration
(5) The accumulation of Aβ may lead to the microglial accumulation and activation resulting in increases in pro-inflammatory cytokines such as interleukin-1 beta, interleukin-6, and tumor necrosis factor-alpha. These cytokine increases in the brain can subsequently lead to tau hyperphosphorylation and a pathological cycle of increased Aβ deposition and persistent microglial activation, ultimately resulting in chronic neuroinflammation and neurodegeneration.
5. Are you aware of pharmacological and non pharmacological interventions to treat such a patient and what are their known efficacies based on RCT evidence?
Ans:
PHARMACOLOGIC:
Cholinesterase inhibitors:
Donepezil
Rivastigmine
Galantamine
NMDA antagonist:
Memantine
NON PHARMACOLOGIC:
Counselling the patient and care givers
Geriatric care
Cognitive / emotion oriented interventions
Sensory stimulation interventions
Behaviour management techniques
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4676992/
NO7)
1) 22yrs old male presented vth c/o intermittent tonic type of seziure since 2months , along vth h/o fever low grade on and off, weight loss,dec appetite.
On/e: pt having lft supraclavicular lymphadenopathy, vth lft axillary lymphadenopathy vth dec breathsounds on lt side
Mri shows- ring enhancing lesions in lt cerebellum region
Could be the possibility of ? TUBERCULOMA
Primaryfocus from lung has to be confirmed vth sputum studies report..
Hiv status of the pt??
It results from the hematogenous dissemination of Mycobacterium tuberculosis from disease elsewhere in the body and the formation of small subpial and subependymal foci in the brain and spinal cord. In some individuals, these foci rupture and release bacteria into the subarachnoid space, causing meningitis.
Magnetic resonance spectroscopy of normal brain shows predominant peaks of N-acetylaspartate (NAA), choline, creatinine and myo-inositol with the highest peak being NAA. NAA is a healthy neuronal marker, choline represents energy store and choline is a marker of cellular turnover
Magnetic resonance spectroscopy is of great value in the diagnosis of tuberculoma in cases of ring-enhancing lesions on CT scan or MRI imaging. It demonstrates a very high lipid peak, reduction in NAA and creatinine and a choline/creatinine ratio of >1 Lipid peak in MRS in the context of a ring-enhancing lesion is very much specific for tuberculoma and has not been seen in any cases of NCC, the other common differential diagnosis of a ring-enhancing lesion. NCC demonstrates a high lactate and proteins like alanine, succinate, glutamate, glycine levels with some reduction of NAA and creatinine A high choline peak is seen in MRS in case of tumors, primary or secondary, because of very high cellular turnover. MRS can also differentiate tuberculoma or tuberculous brain abscess from pyogenic brain abscess by the presence of elevated levels of amino acid peaks in pyogenic brain abscess.
2)
3)A paradoxical clinical worsening of a known condition or the appearance of a new condition after initiating antiretroviral therapy in HIV-infected patients is defined as immune reconstitution inflammatory syndrome (IRIS).BHIVA has issued guidelines[11] for starting the TB treatment with HAART. If CD4+ count is less than 100 cells/μl, both anti-tuberculosis drugs and HAART can be started together. If CD4+ cells are in the range of 100-200; HAART is started 2 months after starting TB treatment. If the CD4+ cells are above 200, HAART is started 6 months after completing TB treatment.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3221202/#!po=6.25000











Comments
Post a Comment